 While it’s possible we could get an Ebola case in Australia, the chances are pretty low, with no direct flights between here and the west African countries most affected.
While it’s possible we could get an Ebola case in Australia, the chances are pretty low, with no direct flights between here and the west African countries most affected.
Those countries also now have in place Ebola screening at their airports. But as Rod Lyon notes in his recent post: ‘most Ebola victims aren’t travelling anywhere fast’.
So the good news is that the likelihood of Ebola overwhelming our health system here is low: it would be simple fear-mongering to suggest otherwise.
Even though Ebola poses little risk to our general population, Australia’s Chief Medical Officer has said that our facilities would be able to contain any cases here and prevent it from spreading further: ‘We have a tried and true system in relation to our quarantine officers… and our health system is really well-placed to manage where there is a concern of a disease of this nature’.
Queensland’s chief health officer recently said Australia’s Ebola preparations had been successfully trialed three weeks ago. A Gold Coast man claimed to be sick on the back of a visit to the Democratic Republic of the Congo in central Africa, hit by a separate outbreak of the disease. He was found not to have Ebola.
But being able to treat an isolated case of Ebola here wouldn’t provide the most accurate assessment of the ability of Australia’s health-care system to respond to a widespread infectious disease outbreak. If a large-scale influenza pandemic occurred in Australia, for example, and spread more quickly than anticipated, then the surge capacity of our health response systems would almost certainly be rapidly overwhelmed.
We still don’t think enough in this country about our public-health system’s need to develop surge capabilities to handle a large influx of patients over a short period of time and our ability to provide adequate care for persons with special medical needs.
There’re no minimum standards for national disaster planning that relate, for example, to the number of critical-care beds or operating theatres required. No hospital sets aside intensive-care-unit beds: instead they rely on rather vague notions of making beds or space available depending on the disaster case load.
The Bali bombings didn’t really test the system: the small number of patients was easily absorbed, and the same applies for victims of the Black Saturday bush fires in Victoria.
Most of our health-care facilities are now operating at close to their maximum capacities, and hospitals have fewer resources for preparedness in harsh financial times.
So the first take–away from the Ebola outbreak is that it reminds us that we need to ensure we’ve got a robust public-health system that can adapt to the challenges that an infectious disease outbreak might pose at home.
The second lesson from the Ebola case stems from Rod’s point that ‘countries that already have strong health systems are better placed to respond to Ebola’. He’s right: so it makes perfect sense that we should help other countries not only to fight specific diseases like malaria and HIV but to build up their public-health infrastructure. That’s the best way we will help in preventing infectious diseases from reaching us, and keeping our public safe.
The third lesson of the Ebola case for Australia arises from Rod’s point that there’s a legitimate concern about the prospect of ‘diseases without borders’, given the ‘growing viral superhighway that globalisation provides’.
The key point here is one that an Australian parliamentary report into health issues across international borders highlighted last year: a disease outbreak in one country can easily spread to another, so we’ll need to have open lines of communication with health officials in different countries to share information for effective disease surveillance.
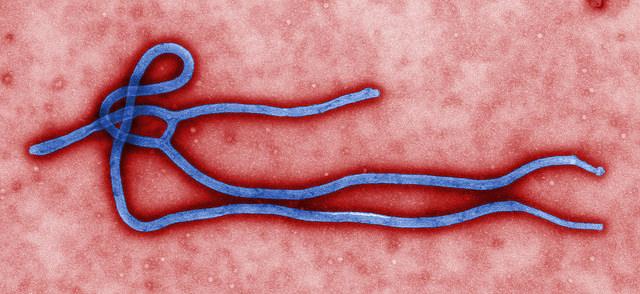
Anthony Bergin is deputy director of ASPI. Image courtesy of CDC Global.