 Synthetic biology is the stuff of dreams and nightmares. Oil-producing algae? Synthetic biology can help. Artificial life? Ask Craig Venter; he’s building his own. Poliovirus cooked up in a test tube? That’s nasty—but too late, in fact; we’ve been there, done that.
Synthetic biology is the stuff of dreams and nightmares. Oil-producing algae? Synthetic biology can help. Artificial life? Ask Craig Venter; he’s building his own. Poliovirus cooked up in a test tube? That’s nasty—but too late, in fact; we’ve been there, done that.
In national security circles, the call is to be alert but not alarmed. It’s very difficult to reverse-engineer viruses like polio. A terrorist group or lone wolf would find it almost impossible. Just as reliable nuclear weapons can only be constructed by well-resourced teams, intricate genetic engineering requires advanced equipment and teamwork. More importantly, it’s hard to acquire the requisite technical know-how on the sly. Of course, that doesn’t stop state action, accidents, theft or loss, unforeseen consequences, or disgruntled insiders wreaking havoc—but it constrains the threat landscape.
Now, however, the biosciences are transforming. Genetic technologies like CRISPR are disruptive, allowing ever more control over the genome. Concurrent advances in bioinformatics and machine learning enable rapid progress. Amateurs are trying DIY-bio in the kitchen, or gravitating towards community ‘biohacking’ spaces like Melbourne’s BioQuisitive. Chances to learn on the internet abound, while scientific literature is becoming more open.
That all drives the diffusion of gene-editing technologies through society. And it explains the appearance of genome editing in the US Director of National Intelligence’s unclassified Worldwide Threat Assessment (PDFs, 2016 and 2017). In fact, the 2016 report names genome editing in the WMD and proliferation category, alongside threats like the North Korean missile program, Syrian chemical weapons and China’s nuclear modernisation.
With the aim of joining a few dots, what follows is a brief case study focusing on an outbreak of disease in Wisconsin last year.
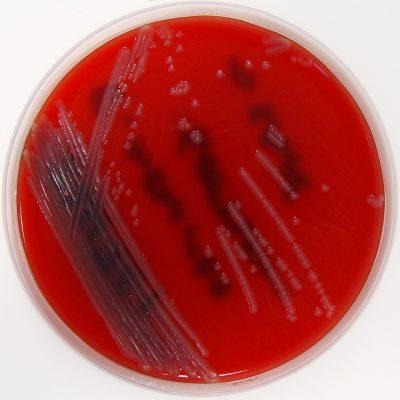
In the 1950s, pioneering biologist Elizabeth O. King identified a genus of bacteria now called Elizabethkingia in her honour. One species, common in the environment and especially in soil and water, was first found in the gut of the Anopheles mosquito. Elizabethkingia anophelis rarely causes human illness. But when infection occurs, it causes meningitis or severe problems in immunocompromised individuals. The US Centers for Disease Control and Prevention (CDC) indicate that around five to 10 cases per state are reported each year.
Beginning in the first half of 2016, 63 Elizabethkingia infections were confirmed in Wisconsin, with 18 fatalities. As per CDC procedures, non-infected individuals who had been treated near infected individuals were swabbed for E. anophelis. All tested negative, suggesting that the infection was not spread within a hospital, as might have been expected.
It seems that a quiet bug had become much more virulent—and that was down to plain evolutionary bad luck. Scientists sequenced the genome of the offending strain, later reporting that a large mutation had disrupted a single gene known as mutY. That gene codes for a protein that repairs DNA, and with the gene disabled, the repair mechanism could not function. In turn, that opened the door for subsequent mutations, boosting the bacteria’s adaptability and ability to disperse; the E. anophelis strain demonstrated ‘hyper-mutagenesis’ and worrying resistance to some common antibiotics.
The outbreak is a vivid example of genome alteration in an existing pathogen. That alteration was caused by blind chance. But gene-editing techniques can readily effect single-target mutations. In a similar setting, a small tweak could be shepherded, deliberately or accidentally, into something more virulent—it would be easier than synthesising a virus from scratch.
And one last point: although researchers could map the genetic changes in the strain, they were unable to pinpoint its geographic origin. There was evidence that the mutY disruption had occurred a year prior to the outbreak; it’s likely that the strain incubated for a time in a product or some other vector, and was later distributed unwittingly throughout the outbreak area. Moreover, it’s possible to make small genetic tweaks that are ‘indistinguishable from naturally occurring genetic variation’. Without proper attribution, a deadly pandemic is more difficult to manage. For hostile actors, that’s appealing.
We worry a lot about custom-built bioweapons and mad scientists, and about ‘gain-of-function’ studies that make deadly viruses deadlier. Experts talk about the possibility that dual-use research will be misused. The US heavily regulates research involving 15 of the deadliest biological agents for that reason. There’s a lot of discussion about explicit and tacit knowledge; knowledge that can be self-taught versus knowledge that cannot. That all makes sense—Frankenstein viruses are the stuff of horror stories, and it’s important to understand how realistic that prospect might be, even if the answer suggests ‘not very’. But we talk less about what might prove to be the real bogeyman—a souped-up superbug modified from hitherto unassuming environmental pathogens.
E. anophelis and other nasties are found in the dirt around us—not in a BSL-4 containment facility. As more people gain access to technologies like CRISPR, and as those techniques become cheaper and more powerful, a simple numbers game suggests we may be headed for an unfortunate intersection.
There are important public health lessons to learn from the Wisconsin outbreak. From a national security viewpoint, however, the incident should prompt questions from policymakers and scientists alike. How difficult is it to identify and delete genes like mutY? Could it be done in open-access neighbourhood labs? And, knowing that the genetic genie can’t be rebottled, how can this prospect be policed?
The emergence of a virulent E. anophelis strain should caution us that the level of sophistication needed for accidental or purposeful misuse of genome editing is less than might sometimes be thought. The proliferation of gene-editing technology should tell us that the barrier is only getting lower.